What is Glaucoma?
Glaucoma has been rightly called the “The silent stealer of eyesight”. The loss of vision is so gradual from along the periphery of the eye that the patient is largely unaware of the loss. What is most tragic is that vision loss due to glaucoma is irreversible. Medication and surgery can at the best preserve the remaining eyesight of the patient.
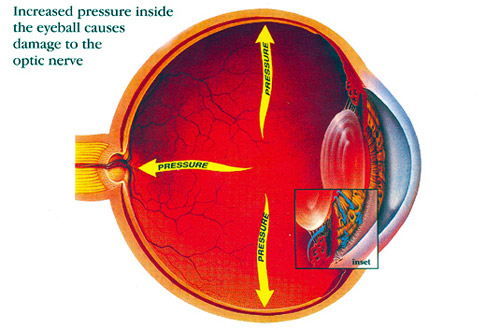
Glaucoma is a result of build up of fluid within the eye and the resultant increase in pressure. This pressure falls on the sensitive optic nerve resulting in irreversible damage.
Types of Glaucoma
Chronic Open Angle glaucoma
As there are hardly any symptoms, the patient is largely unaware that there is a progressive loss of vision. The only way of diagnosis is through periodic eye examinations.
Congenital Glaucoma
This is visible literally from birth. Since the eye of an infant is more elastic than that of an adult, the increase of pressure leads to the eye bulging out.
Acute Angle Closure Glaucoma
This is a sudden onset. Blurred vision, severe pain, rainbow haloes around light, nausea and vomiting are the immediate symptoms. Unless medical attention is provided immediately, blindness can result in a day or two.
Anybody over the age of 40 years is susceptible to Glaucoma. That’s why it is advised that people above 40 should go in for an ophthalmologic examination every 6 months.
Remedies
Glaucoma is usually controlled with eye drops or oral medication given in various combinations. These medications act to decrease the eye pressure either by assisting flow of fluid outside the eye or by decreasing the amount of fluid entering the eye. If medication is poorly tolerated or not effective in controlling the intra-ocular pressure, surgery is done to create an artificial drainage channel for the fluid to drain out.
Frequently Asked Questions
Q. What is glaucoma?
A. Glaucoma is a disease of the optic nerve wherein the nerve is affected resulting in decreased field of vision and it may lead to blindness.
Q. What causes glaucoma?
The exact cause is not known but there are various risk factors. One risk factor is the Intraocular pressure, it is seen that patients who have higher IOP have greater chances of developing glaucoma.
Other risk factors are family history, age, high myopia, migraine, diabetes, long term steroid use, history of inflammation in the eye, history of trauma to the eye etc.
Q. How would I know I have glaucoma?
Unfortunately glaucoma is a silent disease and may not have any symptoms and until a lot of loss has occurred you may not know you have the disease, therefore it is important for everyone to have periodic evaluation of their eyes.
Q.
How often should I get my eyes checked?
There is no rule, but if you are over 40 years you should have it checked every year. If you are over 50 years every 6 months is a good idea. Of course if you have any risk factor which predisposes you to glaucoma your ophthalmologist may suggest more frequent visits. It is an irreversible process hence early detection is necessary
Q.
Does increased eye pressure mean that I have glaucoma?
Not necessarily. Increased eye pressure means you are at risk for glaucoma, but does not mean you have the disease. A person has glaucoma only if the optic nerve is damaged. If you have increased eye pressure but no damage to the optic nerve, you do not have glaucoma. However, you are at risk. Follow the advice of your eye care professional.
Q.
Can I develop glaucoma without an increase in my eye pressure?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is not as common as open-angle glaucoma
Q.
If I have glaucoma can my family also get it?
A positive family history is a risk factor for developing glaucoma so if you have it it is best for your family members to undergo a comprehensive eye examination to be able to detect the disease.
Q. Can children have glaucoma?
Yes children can have glaucoma. It can be a congenital or developmental glaucoma. And can be present at birth and may develop later on also.
Q. How can I know if my child has glaucoma?
For a young child if he or she has a large cornea, which is not transparent, associated with tearing from the eye and if the child shields his eyes in bright light then consult your ophthalmologist.
Q.
If I get hurt on the eyes, can I develop glaucoma?
Trauma to the eye can lead to glaucoma in various ways. There may be injury to the various parts of the eye like the angle which can lead to high pressures. Also the bleeding after trauma can lead to damage. Uncontrolled inflammation can lead to damage to the outflow structures of the eye.
Q.
Are there different types of glaucomas?
The glaucoma can be broadly classified and primary and secondary glaucomas. Secondary as the name suggests are secondary to some other disease in the eye or the body.
Further these types are subclassified in to open angle and angle closure depending on the configuration of the angle or the outflow pathway of the eye.
Q.
How will I know if I have open angle or closed angle glaucoma?
Your ophthalmologist while examining you will do a procedure known as gonioscopy and can define if the angles are open or closed.
Q. Is there a difference in symptoms of both?
Open angle glaucomas are usually symptom -less. In case of angle closure again there may be no symptoms unless the angle closes and there is a sudden rise of IOP when a patient can experience unbearable pain in eyes and blurring of vision with associated coloured halos. Early treatment can help prevent irreversible damage to the optic nerve.
Q.
What does an examination involve?
When you visit your doctor they would like to understand your complaints and take a history of the same. They would also like to know if similar complaints have been there in the past. If any members of your family members if are suffering from glaucoma, it should be informed to the doctor.
You would also be asked about any systemic disease that you are suffering from and the treatment for the same. History of allergy to any medicine is also elicited and kept as a record.
This would be followed by a vision and IOP check. The doctor will look at your eyes through a special machine known as the slit lamp and will look at various parts of your eyes. The optic nerve is carefully looked at and this may require dilating your pupils at times.
The ophthalmologist may require to do a gonioscopy to look for the status of the eye.
Q. What are the other tests done for glaucoma?
After the clinical examination, the doctor may ask for Visual filed evaluation, pachymetry and Optical coherence tomography with ganglion cell complex evaluation.
Q. What do these tests do? Are they painful?
No, the tests are noninvasive and do not cause pain.
The visual field test involves checking for the retinal sensitivity of your retina and assessing the field of vision of the eye. This also helps in glaucoma diagnosis and evaluating progression of the disease.
OCT looks at the retinal nerve fiber layer thickness of your eyes and compares it to the age matched normal data to determine if the nerve is being damaged by glaucomatous disease process. The GCC looks at the ganglion cell complex and is able to detect disease much earlier.
Q.
Will I have to do the tests again and again?
These tests help to refine and define the clinical diagnosis. So they are done at the initial visits to develop a baseline. Subsequently they help in monitoring the progression of the disease hence the ophthalmologist when see you on follow-up visits may discuss with you the frequency and need for repeating the tests.
Q.
What is the treatment for glaucoma?
There are various modalities of treatment available like medication, lasers and surgery. Your ophthalmologist evaluates the disease process in your eye and will discuss with you the most appropriate modality for your eye.
Q. Will I have to continue my medications life long?
The medications for glaucoma help to decrease the rate of progression of the disease and they need in most cases to be continued for life. Your doctor assesses the progression of your disease and can advise continuation of the medications or surgical intervention as the case may be.
Glaucoma Specialists at SCEH